My Blog
-
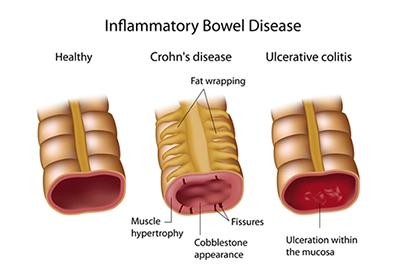
Managing Crohn's Disease Flare-ups
posted: Apr. 22, 2024.

-
Liver Health: Preventive Measures and Lifestyle Changes to Support Liver Function
posted: Apr. 17, 2024.
-
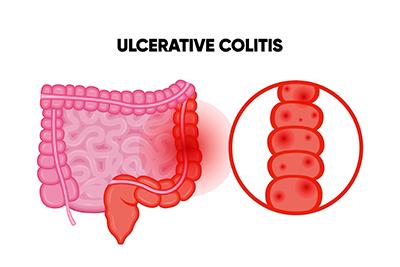
Ulcerative Colitis and Other Digestive Complications
posted: Apr. 01, 2024.
-
Treating Internal Hemorrhoids
posted: Mar. 18, 2024.

-
Three Signs of GERD
posted: Mar. 01, 2024.

-
Are You Dealing With Irritable Bowel Syndrome?
posted: Feb. 15, 2024.

-
Overview of Endoscopy: A Minimally Invasive Diagnostic Procedure
posted: Feb. 03, 2024.

-
Colon Cancer Screening: Understanding Colonoscopies and Other Methods
posted: Feb. 01, 2024.
-
Inflammatory Bowel Disease (IBD): Understanding Crohn's Disease and Ulcerative Colitis
posted: Jan. 16, 2024.
-
What Causes Acid Reflux?
posted: Jan. 01, 2024.

-
Colon Cancer Screening FAQs
posted: Dec. 07, 2023.

-
Don’t Ignore Your Acid Reflux
posted: Dec. 01, 2023.

-
When Is an Endoscopy Needed?
posted: Nov. 09, 2023.

-
The Primary Role of a Gastroenterologist
posted: Nov. 07, 2023.

-
Irritable Bowel Syndrome (IBS): Managing Symptoms and Improving Quality of Life
posted: Oct. 20, 2023.

-
Choosing Us as Your Gastroenterologist
posted: Oct. 10, 2023.

Office Hours
Monday:
8:00 am-5:00 pm
Tuesday:
8:00 am-5:00 pm
Wednesday:
8:00 am-5:00 pm
Thursday:
8:00 am-5:00 pm
Friday:
8:00 am-5:00 pm
Saturday:
Closed
Sunday:
Closed