My Blog
-
The Primary Role of a Gastroenterologist
posted: Nov. 07, 2023.

-
Irritable Bowel Syndrome (IBS): Managing Symptoms and Improving Quality of Life
posted: Oct. 20, 2023.

-
How Your Diet Can Trigger Crohn's Disease
posted: Jul. 27, 2023.
Crohn’s disease affects the gastrointestinal system and how it functions. There isn’t a cure for Crohn’s disease but there are many ways that you can manage your symptoms. One of Read more -
Is Irritable Bowel Syndrome Common?
posted: Apr. 28, 2023.
Irritable bowel syndrome (IBS) is very common and affects about 15 percent of Americans, although IBS symptoms are often mild, if you struggle with them on a regular basis then Read more -
Common Dietary Triggers of Digestive Issues: Identifying and Managing Your Triggers
posted: Mar. 23, 2023.

-
Colon Cancer Prevention: Identifying Warning Signs and Reducing Your Risk
posted: Mar. 14, 2023.

-
What is Crohn's Disease?
posted: Mar. 09, 2023.
Crohn's disease is a chronic inflammatory disorder primarily affecting the gastrointestinal tract. It causes inflammation and damage to the lining of the digestive system, leading to numerous symptoms, including abdominal Read more -
Common Gastrointestinal Disorders and Their Treatments
posted: Feb. 08, 2023.

-
The Benefits of Early Detection: How Colon Cancer Screening Can Save Lives
posted: Jan. 26, 2023.

-
Gastroesophageal Reflux Disease (GERD): Symptoms, Diagnosis, and Treatment
posted: Jan. 13, 2023.

-
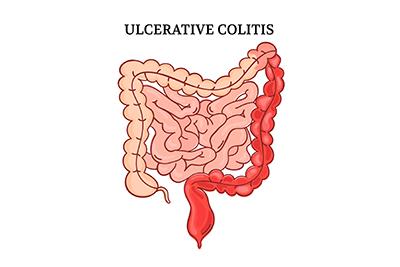
What Is Ulcerative Colitis?
posted: Dec. 28, 2022.
-
What Is an Endoscopy?
posted: Dec. 21, 2022.
Have you been told you need an endoscopy procedure? Wondering what this is and why it is done? We at Digestive Medicine Associates are here to explain. We’re the leaders Read more -
FAQs About Crohn's Disease
posted: Dec. 13, 2022.
Crohn’s disease is a chronic bowel disease associated with inflammation of the gastrointestinal tract. Some patients with the condition experience multiple symptoms, including abdominal pain and cramping, diarrhea, and fatigue. Read more -
Understanding Liver Disease
posted: Dec. 09, 2022.

-
Are You Dealing With Loss of Appetite?
posted: Nov. 23, 2022.

-
Healthy Lifestyle With IBS
posted: Nov. 09, 2022.

Office Hours
Monday:
8:00 am-5:00 pm
Tuesday:
8:00 am-5:00 pm
Wednesday:
8:00 am-5:00 pm
Thursday:
8:00 am-5:00 pm
Friday:
8:00 am-5:00 pm
Saturday:
Closed
Sunday:
Closed